Mastering FHIR Resource Pages: How to Read and Interpret the Patient Resource in Implementation Guides
Introduction to FHIR and Implementation Guides
FHIR is a standard developed by Health Level Seven International (HL7) for the electronic exchange of healthcare information. Utilizing modern web technologies, FHIR is designed to be flexible, scalable, and easy to implement, facilitating interoperability across diverse healthcare systems.
An Implementation Guide (IG) is a set of rules and constraints that customize FHIR resources to meet specific requirements within different contexts, such as regional healthcare systems or specialized use cases. IGs ensure that FHIR resources are applied consistently, adhering to local regulations and operational needs.
Understanding how to read a resource-specific page within an IG is crucial for implementing FHIR effectively. These pages provide detailed information about each resource, including elements, flags, cardinality, constraints, invariants, code systems, and search parameters. For a deeper dive into understanding implementation guides, especially in the Australian context, check out our article on Understanding FHIR Implementation Guides in Australia. If you’re planning to implement FHIR in your organization, our FHIR services can help guide you from strategy to deployment.
Navigating a Resource-Specific Page in an IG
A resource-specific page within an IG, such as the Patient resource page, serves as a comprehensive guide to understanding how that particular resource is structured and utilized within the context of the IG. Here's how to effectively navigate and interpret such a page:
Resource Overview
The description offers a high-level overview of the resource, explaining its purpose and role within healthcare data exchange, while use cases outline typical scenarios where the resource is applicable.
Resource Table
Elements: Lists all the elements (fields) within the resource.
Flags: Indicates special attributes of each element, such as Summary, Must Support, Modifier, Extensions, Constraints, and Invariants.
Cardinality: Specifies how many times an element can appear within the resource.
Code Systems: Details the standardized code systems used for certain elements to ensure consistency.
Element Definitions
Detailed descriptions provide in-depth explanations of each element within a resource, including their data types, possible values, and usage notes. Constraints highlight specific rules or restrictions applied to these elements to ensure proper implementation and adherence to guidelines. Invariants specify conditions that must always hold true for the resource, helping to maintain data integrity and consistency across systems.
Search Parameters
The parameters list enumerates the available search parameters for querying the resource, while usage guidelines provide instructions on effectively utilizing these parameters in search operations to ensure accurate and efficient data retrieval.
Profiles and Extensions
Profiles describe how the resource is tailored to meet specific use cases or regional requirements, while extensions detail any additional elements added beyond the standard specification to address specialized needs.
Examples
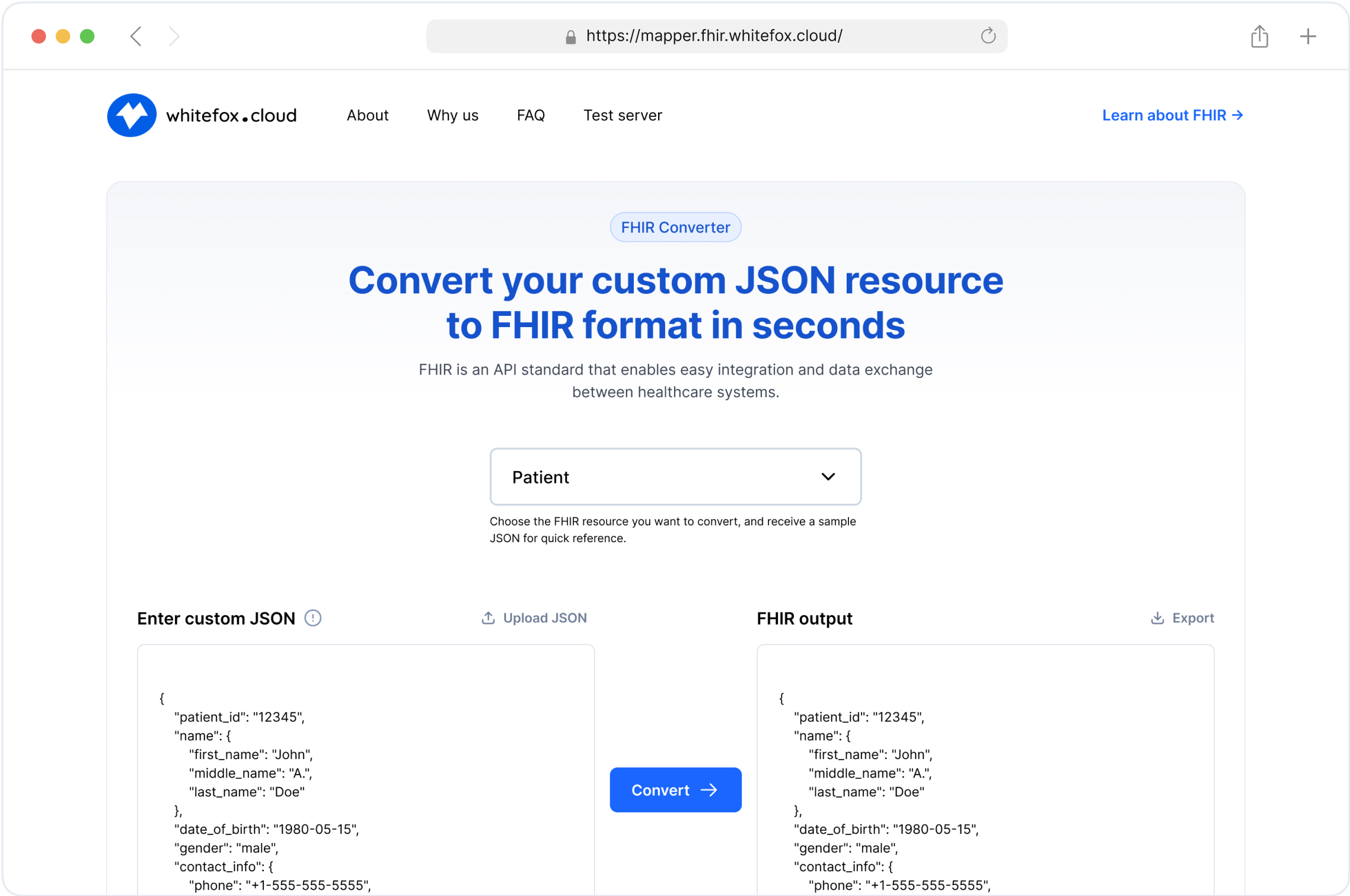
Sample data provides JSON or XML examples that illustrate how the resource is structured, while use cases demonstrate practical applications of the resource in real-world scenarios. You can also try loading these examples into our FHIR test server to see how they behave in practice.
Challenges in Capturing Comprehensive Information on FHIR Resource Pages
Capturing all information from a resource-specific page within an IG can be challenging due to the depth and breadth of details provided. These pages often encompass extensive metadata, numerous constraints, invariants, and a variety of code systems and extensions tailored to specific use cases. For newcomers, the sheer volume of information can be overwhelming, making it difficult to discern which elements are crucial for their specific implementation needs. One way to simplify testing across different profiles is by transforming source data into FHIR-conformant resources first. Our FHIR converter automates this process, reducing complexity when working with multiple IGs.
Key Challenges Include:
Complexity of Details: The intricate explanations of flags, cardinality, constraints, and invariants require a solid understanding of FHIR fundamentals.
Variability Across Profiles: Different IGs (e.g., US Core vs. AU Core) may adapt the same resource in unique ways, necessitating familiarity with multiple profiles.
Dynamic Nature of Standards: FHIR standards and IGs evolve, meaning that information can change, and staying updated requires continuous learning.
Interpreting Extensions: Custom extensions can vary widely between implementations, making standardization and interoperability more complex.
Strategies to Overcome These Challenges:
Incremental Learning: Start by mastering the core elements of the resource before delving into advanced topics like extensions, constraints, and invariants.
Use Visual Aids: Diagrams and tables can help visualize relationships and constraints between different elements.
Leverage Community Resources: Engage with FHIR community forums and participate in discussions to gain practical insights and solutions.
Practical Application: Apply the concepts in real-world scenarios through hands-on projects or simulations to reinforce understanding.
Documentation and Notes: Maintain detailed notes and references to quickly recall complex information when needed.
Understanding Flags in the Patient Resource
Flags within the FHIR Patient resource table provide critical metadata about each element, guiding implementers on how to handle them within different contexts and Implementation Guides (IGs). Understanding these flags is essential for accurate and compliant FHIR implementations.
Summary Flag (∑)
The Summary flag indicates that an element is included in the resource's summary view—a condensed version of the resource containing the most critical elements for quick overviews and lightweight data exchanges. This flag helps reduce the amount of data returned during search operations, enhancing performance and efficiency. Additionally, when a ∑ flag appears in the flags column of a resource table for any element, it signifies that the element will be present in the resource's summary. This ensures that essential information is readily available without the need to retrieve the full resource, facilitating faster data exchanges and streamlined processing.
Implications:
Performance Optimization: Enables efficient data retrieval by focusing on essential elements.
User Experience Enhancement: Facilitates clear and concise information presentation in user interfaces.
Selective Data Exposure: Aligns with privacy and data minimization principles by sharing only pertinent information when comprehensive data is unnecessary.

Must Support Flag (S or SO)
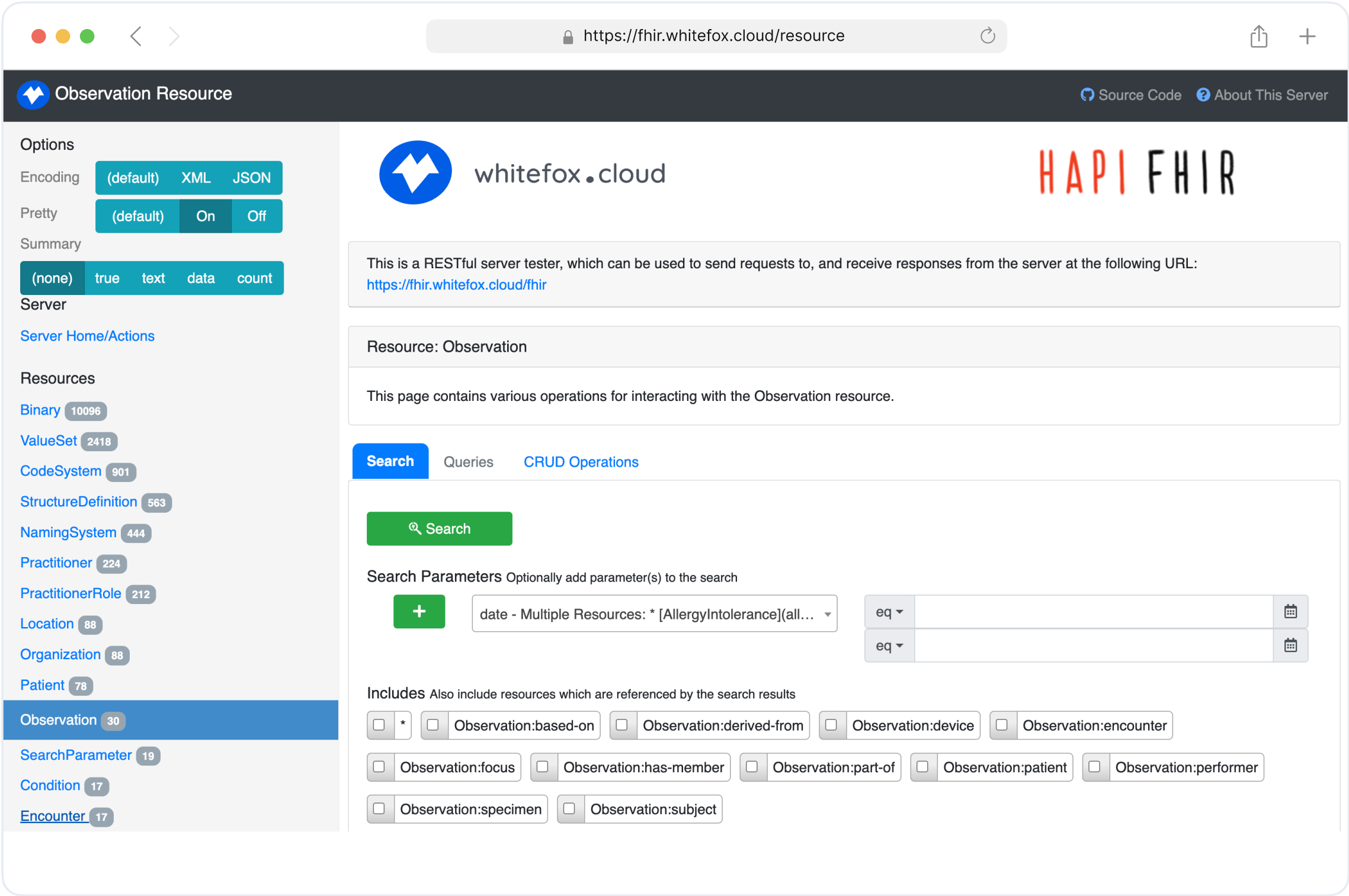
The Must Support flag specifies that an element must be supported by all implementations adhering to a specific FHIR profile within the Implementation Guide. While the element may not be mandatory in every resource instance, systems must be capable of handling it if present. Note that mustSupport is not part of the base FHIR R4 resource definitions but is utilized within profiles to impose additional requirements tailored to specific use cases or regional standards. Developers can validate how these flags affect resource handling by experimenting directly in our FHIR test server.
Implications:
Interoperability: Ensures that all participating systems can process and exchange these elements seamlessly.
Consistency: Maintains a standard level of functionality across different implementations.
Future-Proofing: Allows for the inclusion of additional data elements without disrupting existing workflows.

Modifier Flag (?!)
The Modifier flag designates an element as a modifier element, capable of altering the meaning or interpretation of the containing resource or other elements within it. Modifier elements provide additional context or conditions that influence how the resource should be understood and processed. For example,in the Patient resource the deceased element indicates whether the patient is deceased. If true, it modifies the interpretation of other elements related to the patient's current status.in another word deceasedBoolean as a modifier alters the interpretation of the patient's active status, indicating that the patient is no longer active due to being deceased.
Implications:
Semantic Impact: Modifier elements can change the behavior or interpretation of the resource.
Data Integrity: Systems must recognize and appropriately respond to modifier elements to maintain data accuracy.
Security Considerations: Modifier elements often convey sensitive or conditional information that may affect access controls and data visibility.

Constraints and Invariants Flags (C or I)
The Constraint (C) or Invariant (I) flags indicate that specific elements within an FHIR resource must adhere to defined rules or conditions. These rules ensure that the data remains accurate, consistent, and compliant with both the base FHIR specifications and any additional profiles or implementation-specific requirements.
Properties of Constraints and Invariants:
Key: A unique identifier for the constraint/invariant within its context, used in error messages.
Requirements: The rationale behind the rule and the issues it prevents.
Severity: The importance of the rule violation (Error, Warning, Guideline).
Human Description: A clear, user-friendly explanation of the rule for error messages when the constraint/invariant is not met.
Expression: A FHIRPath expression that must evaluate to true for the element or resource.
XPath: An XPath expression that must evaluate to true for the element or resource in XML representations.
Implications:
Data Validation: Ensures that data meets specific rules beyond basic structure and types.
Consistency: Maintains uniform data quality and structure across different implementations.
Interoperability: Facilitates seamless data exchange by enforcing standardized rules.
Error Prevention: Helps prevent invalid or inconsistent data from being processed or stored.
Severity Levels:
Error (rule): Must be adhered to. Violations should be reported as errors, and the resource can be rejected.
Warning: Indicates potential issues but does not invalidate the resource. Should be reported as warnings.
Guideline: Suggests best practices. Violations should be treated as errors if the implementation context enforces best practices.

Exploring Cardinality in the Patient Resource
Cardinality defines the number of times an element can appear within a resource. It is expressed in the format min..max, where:
min: Minimum number of times the element must appear.
max: Maximum number of times the element can appear (* denotes no upper limit).
Understanding cardinality is crucial for data validation because it ensures data conforms to the specified structure, for implementation because it guides developers on how to handle data input and processing, and for interoperability because it facilitates consistent data exchange across different systems.
A cardinality of 0..1 (Zero or One) indicates that the element can be absent or present once, allowing for optional inclusion while ensuring no duplication. In contrast, 1..1 (Exactly One) mandates exactly one occurrence, guaranteeing that critical information is always provided and preventing missing or multiple instances. A cardinality of 0..* (Zero or Many) permits the element to appear multiple times or not at all, accommodating multiple entries such as various addresses or contact points and thus capturing all relevant instances. Finally, 1..* (One or Many) requires at least one instance but may include more, ensuring a minimum presence while supporting comprehensive data collection.

Code System in FHIR Resource Pages
A code system in FHIR represents a standardized collection of codes used to provide consistency in healthcare data exchange. They define possible values for elements within resources, ensuring that data is interpreted uniformly across different systems. Examples of widely used code systems in healthcare include SNOMED CT, LOINC, and ICD-10 Code Systems.
Code systems are integral to FHIR resources for fields like conditions, medications, procedures, and patient demographics. These systems ensure that healthcare data is not only interoperable but also compliant with global standards.
Key Components of Code Systems in FHIR:
Code: The actual identifier for the concept (e.g., M for Male, F for Female).
Display: A human-readable representation of the code (e.g., "Male," "Female").
Definition: A formal explanation of what the code represents.
URI (Uniform Resource Identifier): A globally unique identifier for the code system.
Here’s a comprehensive example of a FHIR Patient resource illustrating the use of code systems for gender, marital status, and communication preferences in a real-world scenario:

The patient, John Doe, is identified as male (using the HL7 V3 AdministrativeGender code M for "Male") and is married (with the marital status coded as M from the HL7 V3 Marital Status Code System). John communicates in both English and French, with English being his preferred language. The communication preferences reference the HL7 ValueSet for languages, coding English as en and French as fr. This standardized use of code systems ensures consistency and interoperability. For instance, gender is represented as "gender": "male", marital status as "code": "M", "display": "Married", and communication preferences as "system": "http://hl7.org/fhir/ValueSet/languages", "code": "en", "display": "English". By embedding these code systems, healthcare systems across regions can interpret and utilize the data seamlessly. To explore more structured patient examples and validate how code systems resolve, try posting resources to our FHIR test server.
Search Parameters in FHIR Resource Pages
In FHIR, search parameters are predefined criteria that allow clients to query and retrieve specific resources from a server. These parameters can be categorized based on their necessity and support:
Mandatory Search Parameters: These are parameters that a FHIR server is required to support for specific resources, as defined by implementation guides or profiles. For instance, the US Core Implementation Guide specifies certain search parameters that servers must support to ensure interoperability within the US healthcare context.
Optional Search Parameters: These parameters are not required to be supported by all servers but can be implemented to provide additional search capabilities. Their support may vary depending on the server's capabilities and the needs of the implementing organization.
Real-World Example: Patient Resource
Consider a scenario where a healthcare application needs to search for patient records. The FHIR Patient resource offers several search parameters, some of which may be mandatory in certain implementation guides, while others remain optional.
Mandatory Search Parameter Example:
Identifier: A unique identifier assigned to a patient. In some implementation guides, searching by identifier might be mandatory to ensure precise retrieval of patient records. The example query below retrieves the Patient resource with the identifier 12345.
GET [base]/Patient?identifier=12345
Optional Search Parameter Example:
Address: The patient's address details. Support for searching by address may be optional, depending on the server's implementation. The example query below retrieves all Patient resources with an address in Seattle.
GET [base]/Patient?address-city=Seattle
Best Practices for Reading and Implementing FHIR Resource Pages
Start with the Overview: Understand the purpose and scope of the resource within the Implementation Guide (IG) to ensure proper alignment with its objectives. Identify which profiles and resources are included, along with their specific adaptations, to understand their relevance and applicability in your use case.
Examine Resource Tables: Focus on detailed tables that outline each element within the resource, including their definitions, code systems, cardinality, flags, constraints, invariants, and search parameters. Break down each element to comprehend its role within the resource and its significance in data exchange.
Understand Flags, Cardinality, Constraints, and Invariants: Recognize how flags like Summary, Must Support, Modifier, and Extensions influence the handling and interpretation of elements in the resource. Adhere to cardinality constraints to ensure data validity and consistency across systems. Comprehend the rules and conditions enforced by constraints and invariants to uphold data integrity and business logic.
Analyze Profiles and Extensions: Understand how profiles like US Core and AU Core adapt base FHIR resources to meet specific regional or use-case requirements. Use extensions judiciously to add necessary information while adhering to the core structure. Ensure that extensions are well-documented and standardized within the IG.
Pay Attention to Constraints and Invariants: Note specific rules or constraints that govern element usage within the resource. Ensure compliance with these constraints and invariants to align with the IG and meet relevant regulatory requirements.
Utilize Practical Examples: Refer to implementation scenarios to see how resources and profiles are applied in real-world contexts. Use provided JSON or XML samples to understand the data structure and element usage, facilitating accurate implementation.
Refer to Supporting Documentation: Leverage additional references provided within the IG for deeper insights into specific elements, code systems, or usage scenarios. Engage with community forums and HL7 resources for further clarification and support, fostering collaborative learning and problem-solving.
Validate Implementations: Regularly validate your FHIR resources against the Implementation Guide to ensure compliance with all flagged constraints and requirements. Use automated FHIR validation tools to streamline the checking process and confirm adherence to specified structures and rules.
Stay Updated with IG Revisions: Keep track of IG updates and revisions to incorporate new standards and modifications into your implementations. Stay informed about changes to maintain compliance and leverage new features effectively, ensuring that your systems remain up-to-date with evolving healthcare standards.
Automated tools, like our FHIR converter and FHIR test server, make it easier to check compliance with IGs while streamlining data transformations and validation.
Conclusion
Reading and interpreting a resource-specific page within a FHIR Implementation Guide is a fundamental skill for anyone involved in healthcare data exchange and interoperability. Capturing all information from an IG resource page can be challenging due to the complexity and volume of details presented. However, by adopting a structured approach and focusing on key elements like flags, cardinality, constraints, and invariants, professionals can navigate these pages more effectively.
Flags such as Summary, Must Support, Modifier, and Extensions dictate how elements are handled, displayed, and interpreted, shaping system behaviors and data management practices. Cardinality constraints define the structure and repetition of elements, ensuring data consistency and integrity across systems and use cases, while constraints and invariants enforce rules and conditions that uphold data integrity.consistency, and compliance with business logic and regulatory requirements.
Mastery of these concepts not only facilitates effective data exchange but also enhances the overall quality and reliability of healthcare information systems. As the healthcare industry continues to embrace FHIR standards, proficiency in reading and applying resource-specific pages within IGs will remain a valuable asset for developers, implementers, and healthcare professionals alike. To accelerate your FHIR adoption journey, explore our FHIR services and hands-on tools like the FHIR converter and FHIR test server.
Simplify Your FHIR Integration with Our Free Tools
Streamline Your FHIR Implementation
We offer comprehensive FHIR services, from consultation to ongoing maintenance. Our Healthcare Software Development Services