FHIR vs HL7: A Detailed Guide with Practical Examples

Mohammad Reza Tahmaseb
.10 min read
.11 December, 2024
Software Developer
.10 min read
.11 December, 2024
Over the past decades, healthcare has undergone a transformative shift, moving from traditional paper-based records to sophisticated healthcare solutions. This shift has significantly enhanced access to medical information, which was once limited. Historically, healthcare systems faced a major obstacle: the lack of a standardized approach to data exchange. This gap often resulted in fragmented care, limited coordination, and suboptimal patient outcomes.
However, the introduction of standardized protocols brought a revolution, redefining how health data is shared across systems. These standards have enabled healthcare providers to deliver improved patient care, reduce costs, enhance system efficiency, and securely exchange vital information.
Today, HL7 standards are the backbone of global healthcare interoperability, sparking the widely discussed debate of "FHIR vs. HL7." This isn't just a technical conversation—it's a story of evolution, where healthcare moved from isolated systems to connected networks that speak a common language.
In this discussion, we'll explore the journey of healthcare standards, distinguishing HL7 from FHIR, and showing how these advancements have paved the way for a modern healthcare ecosystem. By making health data accessible and exchangeable, we've built a system grounded in the principles of interoperability, shaping the future of healthcare for the better.
1. Introduction
In healthcare, efficient data exchange is crucial for delivering high-quality patient care. FHIR (Fast Healthcare Interoperability Resources) and earlier HL7 (Health Level Seven) are two key standards facilitating healthcare data interoperability, but they serve different purposes and have unique capabilities. This article delves into the distinctions between HL7 and FHIR, offering practical examples to illustrate their applications and help you decide which standard best meets your needs.
2. Understanding HL7 and FHIR
2-1. FHIR and HL7, Related but Distinct Terms:
HL7 (Health Level Seven) is an organization and a broader set of healthcare interoperability standards that facilitate electronic data exchange within healthcare systems. HL7 International develops various standards, with the goal of making it easier for different healthcare systems to communicate and share data effectively.
FHIR (Fast Healthcare Interoperability Resources) is one of the specific standards developed by HL7
This is the timeline in which HL7 developed its standards:

2-2. What Are HL7 Standards?
HL7 (Health Level Seven) standards are a set of international guidelines and frameworks designed to enable the exchange, integration, sharing, and retrieval of electronic health information. These standards are widely used in healthcare to ensure that different healthcare systems and software applications can communicate effectively, thereby improving interoperability and the delivery of healthcare services. HL7’s most well-known protocols are V2, V3 and CDA:
HL7 V2 (1989) : A flexible, text-based messaging protocol widely adopted for data exchange within hospital systems. It includes defined segments for fields such as patient ID, lab results, and medication orders.
HL7 V3 (2003): Developed to bring more structure, it uses XML for improved data consistency but is more complex and less widely adopted than V2.
HL7 CDA (Clinical Document Architecture, 2005): A standardized framework under HL7 for creating and exchanging clinical documents in an XML format. CDA provides a common structure for documents like discharge summaries and progress notes, ensuring that clinical content is both human-readable and machine-processable across systems.
HL7 FHIR (Fast Healthcare Interoperability Resources, 2014): A next-generation standard developed by HL7 for exchanging healthcare information. FHIR is designed to leverage modern web technologies such as RESTful APIs, JSON, and XML, making it scalable, lightweight, and easy to implement. It combines the best features of previous HL7 standards (V2, V3, and CDA) with a focus on flexibility and rapid deployment. FHIR supports a wide range of use cases, from clinical data exchange to mobile health applications, enabling real-time interoperability and seamless integration across diverse healthcare systems.
HL7 serves as the backbone of data exchange in many healthcare facilities, especially where legacy systems are in use.
2-3. What Is FHIR? A Closer Look into HL7's Modern Standard

FHIR (Fast Healthcare Interoperability Resources) is a newer standard introduced by HL7 International in 2014 to address the challenges posed by legacy systems and to support modern web-based applications. FHIR is designed around a RESTful API approach, using JSON, XML, and RDF for data representation.
FHIR’s resource-based structure allows for modular and web-friendly healthcare data exchange. It simplifies complex data by breaking it down into reusable “resources” (e.g., Patient, Observation, Medication) that can be combined to form a complete healthcare record. This design makes FHIR ideal for mobile apps, patient portals, and other cloud-based solutions that require real-time data access. Discover how WhiteFox supports healthcare companies with expert FHIR services, delivered by seasoned professionals.
3. Key Differences Between HL7 Standards
Understanding the key differences between HL7 standards can clarify their respective strengths and limitations.
HL7 standard | HL7 – V2 | HL7 – V3 | HL7 – CDA | HL7 – FHIR |
|---|---|---|---|---|
Structure Type | Message | Structured Message | Document | API-based |
Primary Use | Exchange of medical records | Exchange of medical records | Clinical document sharing | Universal health data exchange, including medical records, patient data, provider info, and wearables |
Supported Platforms | EMR, EHR, HIS | EMR, EHR, HIS | EMR, EHR, HIS | EMR, EHR, HIS, mobile apps, wearables |
Adaptability | Highly flexible | Limited flexibility | Limited flexibility | Extremely flexible |
Data Format | Character-delimited (pipe/hat symbols) | XML | XML | XML/JSON[1] , RDF accessible via API |
Interoperability | Syntactic | Syntactic and Semantic | Syntactic and Semantic | Syntactic and Semantic |
Security | Uses transport layer security | Uses transport layer security | Uses transport layer security | Enhanced security with transport layer security and SSL |
ICD Integration | Limited support | Embeds ICD as an object | Embeds ICD as an object | Embeds ICD as an object |
LOINC Integration | Limited support | Embeds LOINC in RIM object | Embeds LOINC in RIM object | Embeds LOINC in RIM object |
DICOM Integration | Limited support | Embeds DICOM in RIM object | Embeds DICOM in RIM object | Embeds DICOM in RIM object |
Reliability | Less reliable due to optional fields | More reliable with required data fields | More reliable with required data fields | Highly reliable, with specific resources to manage data |
Implementation Cost | Low | High | Moderate to High | Low[1] (new systems); Moderate to High (legacy integration) |
Adoption | Widely used | Less widely used | Widely used | Emerging rapidly as a leading standard |
Learning Time | Short | Long | Moderate | Short to Moderate |
4. Practical Examples of Earlier HL7 Standard (HL7 v2) and FHIR in Action
Example 1: Lab Test Orders
HL7 v2 Approach: In an HL7 v2 system, a lab order might be processed with an HL7 V2 message where each message segment represents a specific part of the order (e.g., patient details, test type, specimen). The lab system receives and decodes the message to extract the information needed to fulfill the order.
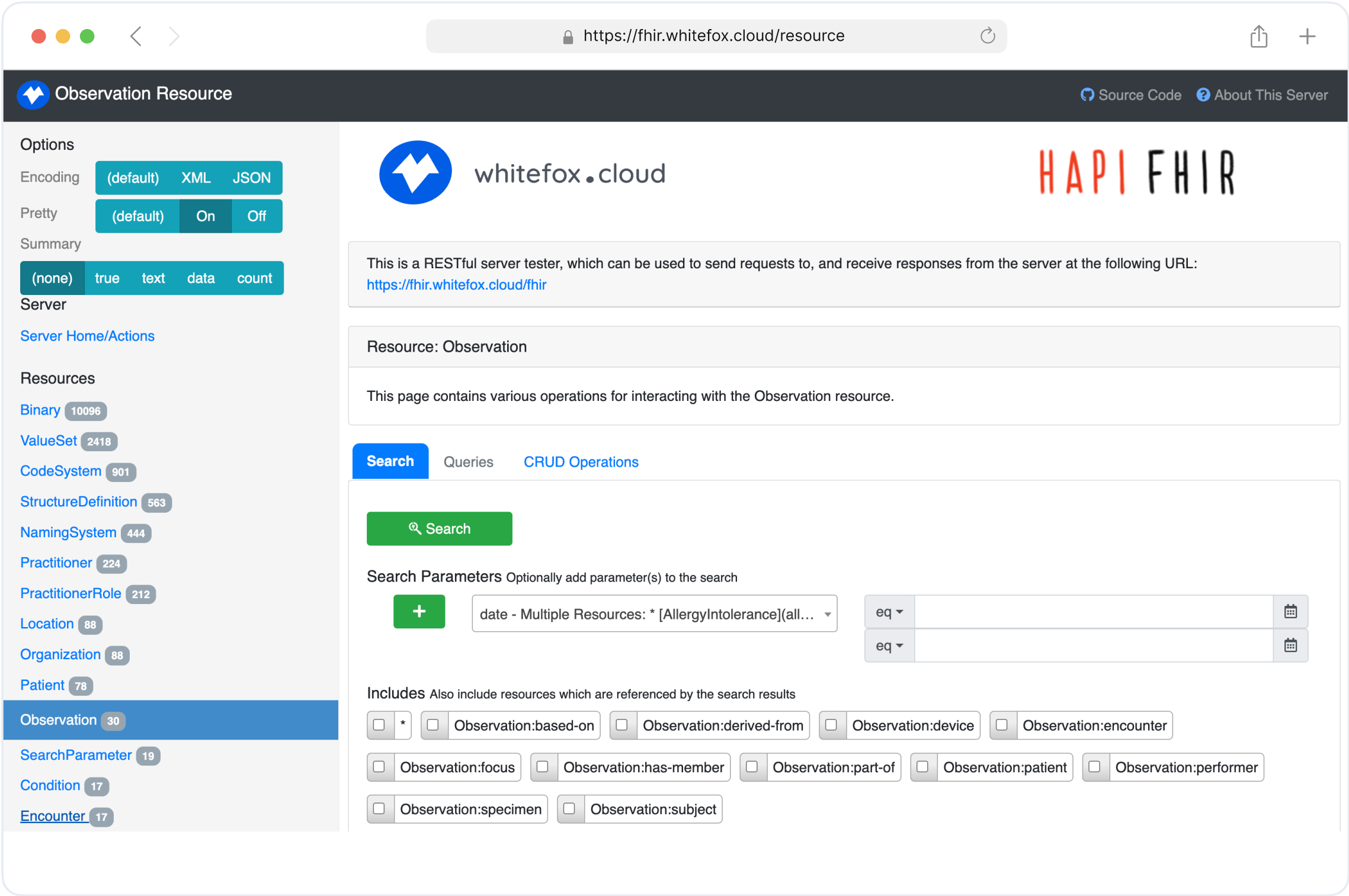
FHIR Approach: In contrast, a FHIR-based system would use a RESTful API call to submit a ServiceRequest resource. The lab application retrieves only the necessary resources, such as Patient and Observation, and updates the order in real-time with minimal processing overhead. To experiment with these scenarios hands-on, you can connect to our FHIR test server and practice sending ServiceRequest, Patient, or Medication resources in real time.
Example 2: Medication Update
HL7 v2 Approach: For medication updates, an HL7 v2 message containing the medication order details is sent from one system to another. Fields like drug name, dose, frequency, and route are embedded in the message and require parsing.
FHIR Approach: FHIR enables easy retrieval and updating of individual fields through its Medication resource. Using a RESTful call, an application can update a patient’s medication in real-time, providing instant feedback to clinicians and patients.
Example 3: Patient Portal Integration
HL7 v2 Approach: Legacy patient portals might pull data from various HL7 V2 messages, aggregating lab results, medications, and appointments into a comprehensive view. However, data synchronization and integration complexity make this challenging.
FHIR Approach: FHIR simplifies portal integration by providing structured, standardized resources like Patient, AllergyIntolerance, and Appointment. These resources can be queried and displayed directly in the portal, improving data consistency and the user experience.
5. Benefits and Limitations of HL7 Standards
HL7 v2
Benefits: HL7 v2 is widely adopted globally and is known for its simplicity and flexibility. It is particularly effective for real-time, event-driven communication, such as patient admissions and lab orders, and is supported by numerous tools and experienced developers.
Limitations: Its flexibility often leads to inconsistent implementations with custom extensions (Z-segments). It lacks modern features like APIs, uses outdated delimited text formats, and struggles with semantic precision.
HL7 v3
Benefits: HL7 v3 offers a structured and rigorous framework based on the Reference Information Model (RIM), enabling detailed and precise data exchange with robust support for terminologies like SNOMED CT and ICD.
Limitations: Its complexity, steep learning curve, and high implementation costs have limited its adoption. The rigid and abstract design makes it less flexible and difficult to adapt to specific needs.
CDA (Clinical Document Architecture)
Benefits: CDA is widely used for clinical document exchange, providing both human-readable narratives and machine-readable structured data. It simplifies document sharing for use cases like discharge summaries and progress notes.
Limitations: It is limited to document-centric use cases and inherits the complexity of HL7 v3. Its static nature makes it unsuitable for real-time, dynamic workflows.
FHIR (Fast Healthcare Interoperability Resources)
Benefits: FHIR uses modern web technologies like RESTful APIs, JSON, and XML, making it flexible, easy to implement, and ideal for new systems. It offers modular resources and is rapidly becoming the leading standard for healthcare interoperability.
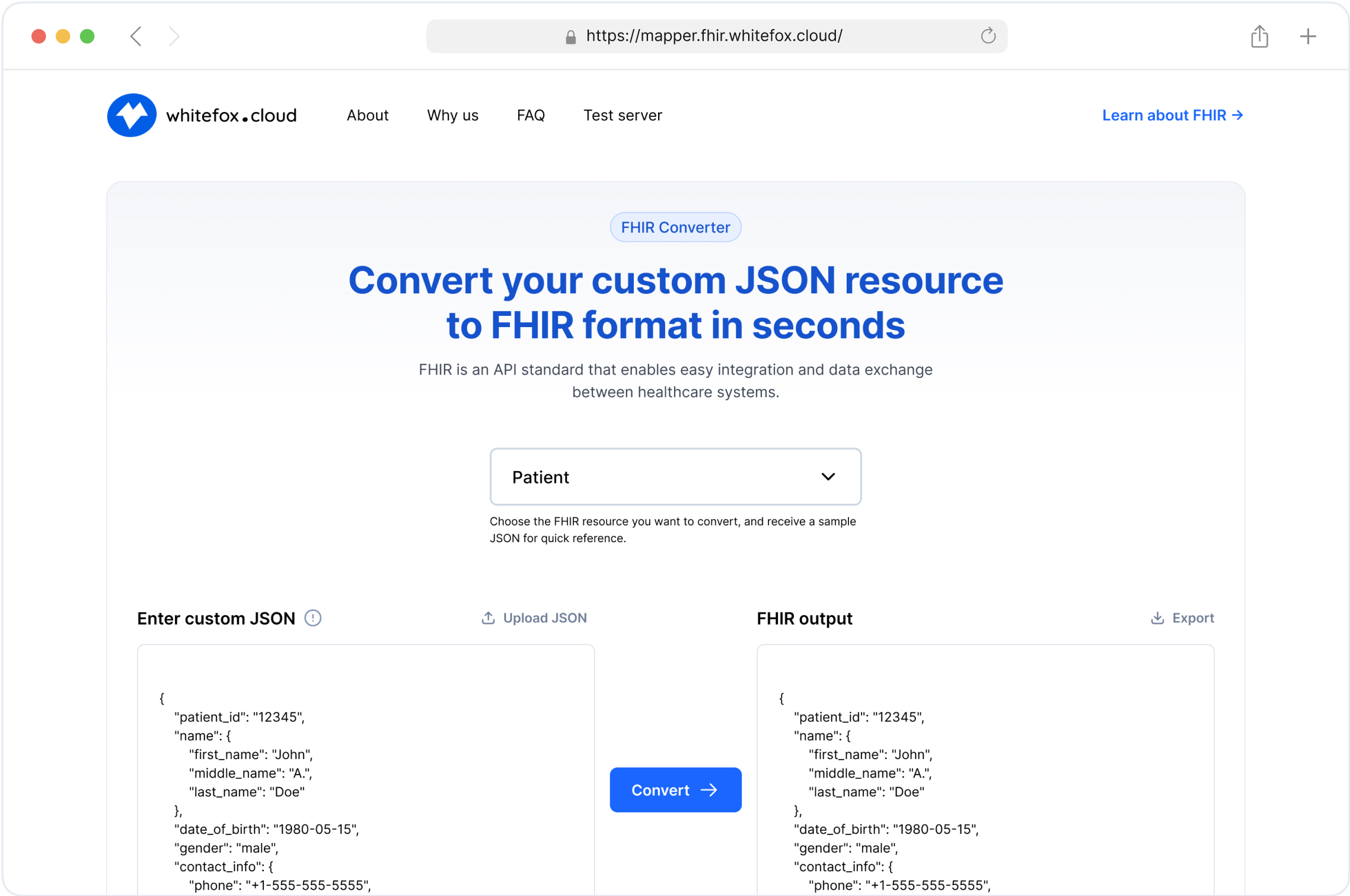
Limitations: FHIR is still evolving and less mature for complex use cases. Integration with legacy systems like HL7 v2 can be challenging, and implementation consistency across vendors is not yet fully standardized. Tools like our FHIR converter help bridge that gap by transforming HL7 v2/v3 messages into valid FHIR resources.
6. How to Communicate with HL7 Standards
Lets see how each systems messages looks like:
HL7 (v2) : HL7 v2 messages are delimited by pipes (|), and segments start with a segment identifier.

HL7 (v3) : HL7 v3 messages are XML-based and more verbose than v2. Below is a simplified example.

HL7 (CDA) : HL7 CDA messages are document-based. Below is a simplified example.

FHIR : FHIR messages are typically RESTful and JSON-based. Here's a sample Patient resource.

7. Compare the Adoption of HL7 Standards Across Different Countries
HL7 standards adoption varies widely across countries, influenced by unique healthcare system needs, government regulations, and interoperability priorities. Here’s a comparative look at HL7 V2, V3, and FHIR adoption across regions:
United States:
HL7 V2: Widely used in hospitals and health systems for internal messaging.
FHIR: Strongly encouraged by government regulations like the 21st Century Cures Act, promoting patient data access and interoperability.
European Union:
HL7 V2: Used in many countries for internal messaging within healthcare organizations.
FHIR: Increasingly adopted, with strong uptake in the Netherlands and Sweden for cross-border data sharing and digital transformation, supported by initiatives like MyHealth@EU.
Australia:
HL7 V2: common in hospitals.
FHIR: Actively adopted in national projects like My Health Record, aimed at improving patient data interoperability.
Learn more about FHIR Implementation Guides in Australia
Canada:
HL7 V2: Widely implemented; HL7 V3 saw limited success.
FHIR: Now promoted as the preferred standard for new interoperability initiatives, supported by agencies like Infoway.
New Zealand:
HL7 V2: Traditionally used in healthcare messaging.
FHIR: Growing adoption, with government initiatives supporting patient-centered data exchange.
Brazil:
HL7 V2: Used in some hospital systems.
FHIR: Recently adopted as the standard for the national health data network, Conecte SUS, aiming to modernize healthcare interoperability.
United Kingdom:
HL7 V2: Commonly used within the NHS for legacy systems.
FHIR: A major focus of the NHS’s digital transformation strategy, promoting nationwide interoperability.
Summary:
HL7 V2: A legacy standard still common globally, especially for internal messaging within healthcare systems.
FHIR: Rapidly becoming the preferred standard for interoperability, with strong government support in countries like the U.S., EU nations, Australia, Canada, and others driving digital health priorities.
8. Is FHIR Superior to Earlier HL7 Standards?
FHIR (Fast Healthcare Interoperability Resources) represents the latest standard from HL7, designed to overcome limitations found in previous HL7 protocols. By building on lessons learned and leveraging the strengths of earlier standards, FHIR is tailored to meet the current demands of the healthcare industry for seamless data sharing and system interoperability.
FHIR has clear advantages over its HL7 predecessors:
Easier Implementation: Unlike older HL7 standards, FHIR integrates a broader range of technologies and is simpler to implement, focusing on reducing obstacles for developers aiming for interoperability. Its compatibility with modern web-based tools and programming languages makes it a practical choice for software engineers.
Flexibility for Common Use Cases: FHIR provides modular “resources” that developers can use as building blocks for custom applications. This design gives healthcare developers the adaptability needed to address various operational, administrative, and clinical needs within healthcare organizations.
Free Access to Resources: FHIR is openly accessible, offering all necessary resources at no cost, which significantly reduces the expenses involved in its implementation. This free availability is a valuable asset for organizations looking to adopt a robust standard without incurring high setup costs.
Support for Multiple Architectures: FHIR supports a range of data exchange models, giving developers flexibility in designing solutions that fit complex, multi-layered healthcare systems. This flexibility helps in achieving interoperability across diverse architectures and workflows.
Enhanced Data Control and Security: FHIR offers advanced features for data management, providing patients and healthcare providers more control over shared information. By facilitating secure and straightforward data exchange, FHIR meets today’s stringent data governance needs.
These features make FHIR a strong candidate for healthcare organizations looking to stay adaptable in an environment where interoperability requirements are constantly evolving. Although not without its own challenges, FHIR has emerged as a top choice for developers creating healthcare applications that need to meet modern interoperability standards.
9. How to Choose Between HL7 Standards for Your Organization
Selecting between HL7 standards depends on several factors:
Existing Infrastructure: Organizations with established legacy systems that rely on earlier HL7 standards may benefit from sticking with earlier HL7 standards, especially if budget constraints limit large-scale upgrades.
Need for Modernization: Organizations aiming to support web and mobile access, or those implementing patient-facing applications, should consider FHIR. Our FHIR services provide the frameworks and expertise to guide this modernization process.
Budget and Expertise: Implementing earlier HL7 standards, particularly in V3, can be costlier and more resource-intensive due to its complexity. FHIR, while easier to adopt for new applications, may still require expertise to integrate with legacy systems.
Interoperability Requirements: If interoperability with external systems is crucial, especially cloud or mobile services, FHIR offers the flexibility to meet modern interoperability demands.
10. Conclusion
All HL7 standards play essential roles in healthcare interoperability, but they serve different purposes. Earlier HL7 standards remains indispensable for organizations heavily reliant on legacy systems and serves as a proven standard for in-hospital data exchange. FHIR, however, represents the future of healthcare data exchange, offering an API-friendly, modular solution that aligns with the demands of cloud-based applications and real-time data access.
Choosing between earlier HL7 standards and FHIR depends on your organization’s infrastructure, interoperability needs, and future goals. By understanding their unique strengths, you can make an informed decision to enhance your healthcare data management strategy. To start your own HL7-to-FHIR journey, explore our FHIR services, try the FHIR converter for message transformations, or test implementations directly with our FHIR test server.
11. FAQ
1. What is the difference between HL7 and FHIR?
HL7, as an organization, developed multiple standards over time, including HL7 v2, v3, and CDA, which are collectively referred to as the former HL7 standards. These standards focused on specific use cases, such as messaging (v2), detailed data models (v3), and document exchange (CDA), but often lacked consistency and flexibility, with complex implementations. In contrast, FHIR (Fast Healthcare Interoperability Resources), also developed by HL7, represents a new-generation standard that unifies and modernizes interoperability by leveraging web technologies like RESTful APIs and JSON. FHIR simplifies implementation, supports modular resource-based data representation, and provides broader compatibility with modern healthcare systems, offering a significant improvement over earlier HL7 standards while remaining within the HL7 framework.
2. Is FHIR replacing earlier HL7 standards?
FHIR is not replacing earlier HL7 standards entirely. Older HL7 standards like V2 remain widely used and will continue to be supported. However, FHIR is gaining prominence due to its modern approach, making it the preferred choice for new healthcare applications and interoperability solutions.
3.Is it possible to convert HL7 v2/v3 messages to FHIR resources?
Yes, HL7 messages can be converted to FHIR using tools like the FHIR Converter. This allows organizations to transition from legacy HL7 standards to FHIR for improved data exchange and modern system compatibility.
4. Why is FHIR considered better than earlier HL7 standards?
FHIR is often considered better because it simplifies implementation through reusable resources, supports modern web-based applications, and leverages widely-used technologies like JSON and RESTful APIs. These features enable faster development and enhanced interoperability compared to older HL7 standards.
5. What are the key use cases for the earlier HL7 standard vs. FHIR?
Earlier HL7 standards are ideal for legacy systems and internal hospital communication, while FHIR excels in patient-facing apps, mobile solutions, and real-time data exchange. The choice depends on the organization's infrastructure and interoperability requirements.
6. How is FHIR different from previous HL7 standards?
Unlike earlier HL7 standards, FHIR focuses on modular design with resources like "Patient" or "Observation" that can be easily combined. FHIR also supports RESTful APIs, enabling real-time data exchange and integration with cloud-based systems and mobile applications.
7. Why should organizations consider adopting FHIR?
Organizations should adopt FHIR to stay aligned with modern interoperability standards, enhance patient engagement, and improve system integration. FHIR’s flexibility, ease of use, and support for modern technologies make it a future-ready standard.
8. What are the limitations of earlier HL7 standards compared to FHIR?
HL7’s older standards, particularly V2 and V3, are less flexible and harder to implement for modern use cases. They also lack native support for mobile and web-based applications, making them less suitable for cloud integration and real-time data sharing.
9. Which countries are leading in FHIR adoption?
Countries like the United States, Australia, Canada, and several European nations are leading FHIR adoption. These regions prioritize interoperability and modern healthcare systems, making FHIR the preferred choice for national and cross-border health data exchange.
10. How does FHIR support modern healthcare applications?
FHIR’s RESTful architecture and use of standard web formats like JSON and XML make it perfect for developing modern applications such as patient portals, wearable device integration, and mobile health apps. This capability ensures real-time data access and improved patient experience.
Simplify Your FHIR Integration with Our Free Tools
Streamline Your FHIR Implementation
We offer comprehensive FHIR services, from consultation to ongoing maintenance. Our Healthcare Software Development Services