Unleashing Healthcare Data Silos: How FHIR Advances Interoperability
The Evolution of Interoperability: Tackling Data Silos in Healthcare Systems
In the 1980s, the primary goal of interoperability was to connect different systems (e.g. two distinct systems) within a single hospital, because communication is integral to most healthcare processes. Hospitals began adopting multiple systems that needed to communicate internally. As hospitals integrated more specialized systems across various departments, the issue of disconnection grew more pronounced. For example, when scheduling a surgery, these systems often failed to automatically update the patient's medical history, notify the surgical team, or allocate the necessary operating room. This lack of integration impeded the seamless exchange of information within the hospital. To address this need, Health Level Seven International (HL7) was established, introducing HL7 Version 2 (V2 messaging), a standard for exchanging information between hospital systems.
Today, hospitals might have an average of over 100 IT systems. Data is no longer confined to hospitals; it is also found in payers' systems, patients' mobile devices, home devices, and genomic sequencing labs. This explosion of data presents new challenges. If in 1980, about ten facts were needed for complex healthcare decisions, then by 2020, this number might have increased to around 1,000 facts per decision, while humans can process only about five to nine facts at a time. Clinical decision support systems were an early significant application of informatics in patient care.
Interoperability now means more than just connecting two systems. It involves enabling various healthcare information systems, such as electronic health records (EHRs), pharmacies, lab systems, and imaging software, to connect, exchange data, and collaborate seamlessly. This allows healthcare providers to access and share patient information efficiently and securely, regardless of the specific systems used. Achieving this level of interoperability is challenging due to varying clinical terminologies, technical specifications, and functional capabilities, making it difficult to create a single standard format for sharing data.
The key takeaway is that interoperability has increased significantly over the past decade. Check out Figure 1 to see how U.S. hospitals went from info silos to info sharers. In 2014, only 23% of hospitals met all four of the measured criteria for interoperability. By 2022, that number had jumped to 70%, and it remained steady at 70% in 2023. These criteria include sending summaries of care records electronically, receiving them electronically, finding health information electronically, and integrating electronic health information into their own EHR systems. These findings show a positive trend towards improved information exchange among hospitals, which can potentially lead to better care coordination and patient outcomes.
![Figure 1: U.S. hospital interoperability for sharing patient data electronically (sending, receiving, searching, integrating) soared from 23% in 2014 to 70% by 2023. Gathered from [12].](http://images.ctfassets.net/99vzrxdqm41r/4otdEKYzGnc0U0aBaMIEA0/3809bead722ef695eed74d6294cca1c4/us-hospital-interoperability.png)
The challenges to interoperability include:
Broken Language Barrier:
Imagine different healthcare systems speaking different languages. Without common data formats, interfaces, and communication protocols, exchanging and understanding information becomes a frustrating struggle.
Islands of Information:
Healthcare organizations often operate in silos. Multiple digital systems like EHRs, imaging, labs, and telehealth platforms create isolated data islands, hindering the flow of vital information.
Fort Knox Security:
Healthcare data is like Fort Knox – heavily guarded. Strict privacy regulations are essential, but they also add complexity to secure and controlled data exchange.
Tech Time Warp:
Outdated technology in many medical facilities acts like a time warp, limiting their ability to connect with newer, more integrated systems.
Addressing these challenges requires collaborative efforts among healthcare organizations, technology vendors, standardization bodies, and regulatory agencies.
The Birth of FHIR
Recognizing the limitations of existing standards, HL7 initiated a task force over a decade ago to create a new standard from scratch. Grahame Grieve from Australia introduced the concept of FHIR, designed to address modern data challenges by integrating both narrative (i.e. human displayable form) and coded data.
What is FHIR?
At its core, FHIR is a REpresentational State Transfer (REST) API (Application Programming Interface), which is the foundation of most internet-based data exchanges. RESTful APIs use standard HTTP methods (GET, POST, PUT, DELETE) to interact with resources. For example, GET /Patient/123 to get a patient with ID 123. REST architecture employs statelessness, where client-server interactions are independent. Each client request contains all required information, eliminating the need for the server to store context from previous exchanges. This approach ensures self-contained, efficient communication between client and server.
Similar to travel websites aggregating flight information, FHIR standardizes healthcare data representation and exchange, enabling different systems to communicate seamlessly. In essence, FHIR was designed to assemble a set of resources and create RESTful APIs using HTTP methods to access and control these resources.
Key Concepts of FHIR
1. FHIR Resources
These are the basic units representing various data elements in healthcare. For example, a patient resource includes attributes like given name, family name, date of birth, and gender. Resources also include medications, care plans, and infrastructure elements like lists and rules. By standardizing these resources, FHIR ensures that systems can interpret the data consistently, no matter where it originates. A fundamental characteristic of resources is their ability to link to other resources.
Here's an example of an JSON representation for a patient resource using the FHIR standard.
{
"resourceType": "Patient",
"id": "321",
"active": true,
"name": [
{
"use": "official",
"family": "White",
"given": [
"Owen",
"C."
]
}
],
"telecom": [
{
"system": "phone",
"value": "+1 (123) 123-4455",
"use": "home"
}
],
"gender": "male",
"birthDate": "1997-03-01",
"deceased": {
"boolean": false
},
"communication": [
{
"language": {
"coding": [
{
"system": "http://terminology.hl7.org/CodeSystem/languages",
"code": "en",
"display": "English"
}
]
}
}
],
"extension": [
{
"url": "http://hl7.org/fhir/StructureDefinition/patient-birthplace",
"valueString": "New York City, NY"
}
]
}This example highlights various data elements you can include in a FHIR Patient resource, utilizing standard coding systems to enhance interoperability.
This structure is useful for exchanging patient information in a standardized format across different healthcare systems, ensuring interoperability and easy access to critical patient data.
2. FHIR Profiles
Profiles customize FHIR resources for specific use cases or regions, including vocabulary bindings, extensions, and relationship rules, ensuring data consistency across different systems. For example, a profile for a diabetes management application would include specific data elements relevant to monitoring blood sugar levels, medication schedules, and dietary recommendations.
3. FHIR Terminology Server
This server stores value sets and code systems, making standardized terminologies accessible. For instance, an app managing diabetes care can reference a value set of insulin types on the FHIR terminology server. This ensures that all systems using the app refer to the same set of insulin types, facilitating accurate and consistent treatment.
4. FHIR Extensions
FHIR Extensions enhance the core FHIR standard by allowing the addition of data elements that are not universally applicable, thereby keeping the FHIR framework simple and straightforward for implementation. These extensions are crucial for maintaining transparency and interoperability, as they must be publicly accessible. For example, a hospital catering to international patients might include a "nationality" extension to better manage medical records for patients from various countries.
This mechanism of extensions is rooted in the "80% rule" of FHIR, which acknowledges that while the FHIR standard covers the majority of healthcare data needs, it cannot anticipate every specific scenario across different healthcare sectors. HL7 manages a registry of these extensions to promote reuse and prevent redundancy, enabling healthcare systems to integrate these extensions as needed to meet specific operational requirements. This system ensures that FHIR remains adaptable and responsive to the diverse needs of the healthcare community, from specialized care facilities to broad medical institutions.
5. FHIR Implementation Guide
This comprehensive resource specifies how to construct and use FHIR resources for specific use cases, including profiles, value sets, code systems, and extensions. It's machine-readable, facilitating easy sharing and validation. For instance, an implementation guide for a remote patient monitoring application would detail the required FHIR profiles and data exchange protocols to ensure seamless interaction between patients and healthcare providers.
Implementation Guides and Reference Implementations
Implementation guides like FHIR AU-Core (FHIR AU-Core is a set of guidelines in Australia for how healthcare data should be structured and exchanged) are essential for standardizing healthcare data exchange. They outline how data should be structured to ensure different systems can communicate effectively.
While these guides are crucial, they can be complex. Without a reference implementation—a practical example showing how to apply these guidelines—developers might find it challenging to implement them correctly.
Why Reference Implementations Matter
Clarity:
They help developers understand the guide’s specifications.
Best Practices:
They demonstrate the best ways to implement the standards.
Testing:
They provide a benchmark to ensure solutions meet the required standards.
Having a reference implementation makes it easier for organizations to adopt and correctly use implementation guides like FHIR AU-Core, ensuring better interoperability and more effective data exchange in healthcare.
Why FHIR?
FHIR offers a robust framework for healthcare data exchange that surpasses older standards like HL7 V2 in several key ways, enhancing both the efficiency and flexibility of health information systems.
1. Enhanced Flexibility and Customization
FHIR stands out due to its adaptability, allowing healthcare organizations to define and customize their own data models. This flexibility supports the development of tailored healthcare applications to meet specific organizational needs, a significant step up from the more rigid data model constraints of HL7 V2.x, which can be challenging to alter.
2. Modern and Efficient Technology
FHIR uses modern web technologies such as RESTful APIs, JSON, and XML, which streamline the data exchange process. These technologies facilitate faster and more efficient communication between systems compared to HL7's older methods, making FHIR particularly suitable for today's mobile and web applications. This approach not only simplifies integration with existing systems but also enhances the performance and usability of healthcare apps on mobile devices.
3. Improved Security Protocols
FHIR includes support for contemporary security protocols like OAuth2 and OpenID Connect, enhancing the protection of sensitive healthcare data. This is a major advancement over HL7, which lacks built-in security features, thus requiring organizations to implement their own security measures.
4. Strong Developer Support and Community
FHIR can be utilized without any associated costs, designed with developers in mind, FHIR is easier to implement and integrate into various applications, thanks to its use of familiar web technologies and a clear, logical structure. This ease of use is coupled with a strong community of developers and healthcare professionals who continuously contribute to the evolution of the standard, ensuring it remains relevant as healthcare technology advances.
5. Broad Adoption and Regulatory Support
FHIR has seen widespread adoption across the healthcare industry, including backing from major tech corporations and governmental agencies, which enhances its viability as a long-term standard for health data exchange. Its growing adoption is supported by its alignment with regulatory frameworks aiming to improve healthcare interoperability on a large scale.
6. Real-World Applications
FHIR is not just theoretically beneficial; it is actively improving healthcare IT in various areas. For example, it supports clinical decision systems by providing real-time data access, enables personalized medicine through comprehensive patient histories, and facilitates telemedicine by ensuring reliable and quick data transmission.
In summary, FHIR provides a modern, secure, and flexible framework that addresses the limitations of previous standards like HL7 V2, Clinical Document Architecture (CDA), Digital Imaging and Communications in Medicine (DICOM) and Continuity of Care Document (CCD), making it a leading choice for future-proofing healthcare data exchanges.
The Impact and Future of FHIR
FHIR's machine-readable format and widespread adoption have revolutionized healthcare data interoperability, enabling seamless data exchange and interpretation. While the challenge of plug-and-play applications across different EHR systems remains due to data representation variations, FHIR simplifies creating interoperable solutions within specific environments. For example, FHIR facilitates real-time data sharing between a patient's smartwatch and their healthcare provider's EHR system, allowing for continuous monitoring and timely interventions.
Challenges and Future Outlook
The state of medical records worldwide, especially those still relying on paper, presents significant challenges in healthcare. These records often suffer from disorganization, illegibility, and an abundance of mixed notes and reports, complicating the extraction of essential information for healthcare professionals and ultimately impeding patient care. Efforts to digitize and standardize health information, such as the adoption of FHIR-based APIs in the U.S and U.K., have been slow, leaving many systems reliant on inefficient paper-based documentation.
Despite the many benefits of FHIR, integrating it with legacy systems is complex and resource-intensive, requiring ongoing education and training to keep pace with its evolution. Ensuring stakeholder alignment and commitment to the adoption process is also crucial for success.
The future of FHIR looks promising as it continues to evolve and adapt to the dynamic needs of the healthcare industry. Ongoing collaboration among healthcare providers, technology developers, and regulatory bodies will drive further advancements in FHIR, making healthcare data exchange more efficient, secure, and effective.
Conclusion
FHIR represents a remarkable innovation in healthcare data interoperability, enabling real-time data access across multiple platforms. Its flexibility and standardization will continue to drive future innovations, improving patient care and operational efficiency. As more healthcare systems adopt FHIR, we can expect to see even greater advancements in personalized medicine, remote patient monitoring, and integrated care delivery.
References
Health Level Seven International (HL7). Retrieved from
Surety Systems. FHIR vs. HL7: Your Guide to Healthcare Data Exchange Standards. Retrieved from https://www.suretysystems.com/insights/fhir-vs-hl7-your-guide-to-healthcare-data-exchange-standards/
Relevant Software. FHIR vs. HL7. Retrieved from
HealthIT.gov. Electronic Health Information Exchange (Hospitals). Retrieved from
https://www.healthit.gov/data/quickstats/electronic-health-information-exchange-hospitals
Benson, T., & Grieve, G. (2021). Principles of Health Interoperability: FHIR, HL7 and SNOMED CT (4th ed.). Springer Nature Switzerland AG.
InterSystems. Building Your First HL7 Integration [Course]. InterSystems Learning. Retrieved from https://learning.intersystems.com/course/view.php?id=2327
Braunstein, M. L. (2022). Health Informatics on FHIR: How HL7's New API is Transforming Healthcare. Springer.
Saripalle, R., Sookhak, M., & Haghparast, M. (2020). An Interoperable UMLS Terminology Service Using FHIR. Future Internet, 12(11), 199. https://doi.org/10.3390/fi12110199
Subrahmanya, S. V. G., Shetty, D. K., Patil, V., Hameed, B. Z., Paul, R., Smriti, K., ... & Somani, B. K. (2022). The role of data science in healthcare advancements: applications, benefits, and future prospects. Irish Journal of Medical Science (1971-), 191(4), 1473-1483.
Magnuson, J. A., & Dixon, B. E. (2020). Public Health Informatics and Information Systems (3rd ed.). Springer Nature Switzerland.
Ayaz, M., Pasha, M. F., Alzahrani, M. Y., Budiarto, R., & Stiawan, D. (2021). The Fast Health Interoperability Resources (FHIR) standard: systematic literature review of implementations, applications, challenges, and opportunities. JMIR Medical Informatics, 9 (7), e21929.
HealthIT.gov. Electronic Health Information Exchange (Hospitals). Retrieved from
https://www.healthit.gov/data/quickstats/electronic-health-information-exchange-hospitals
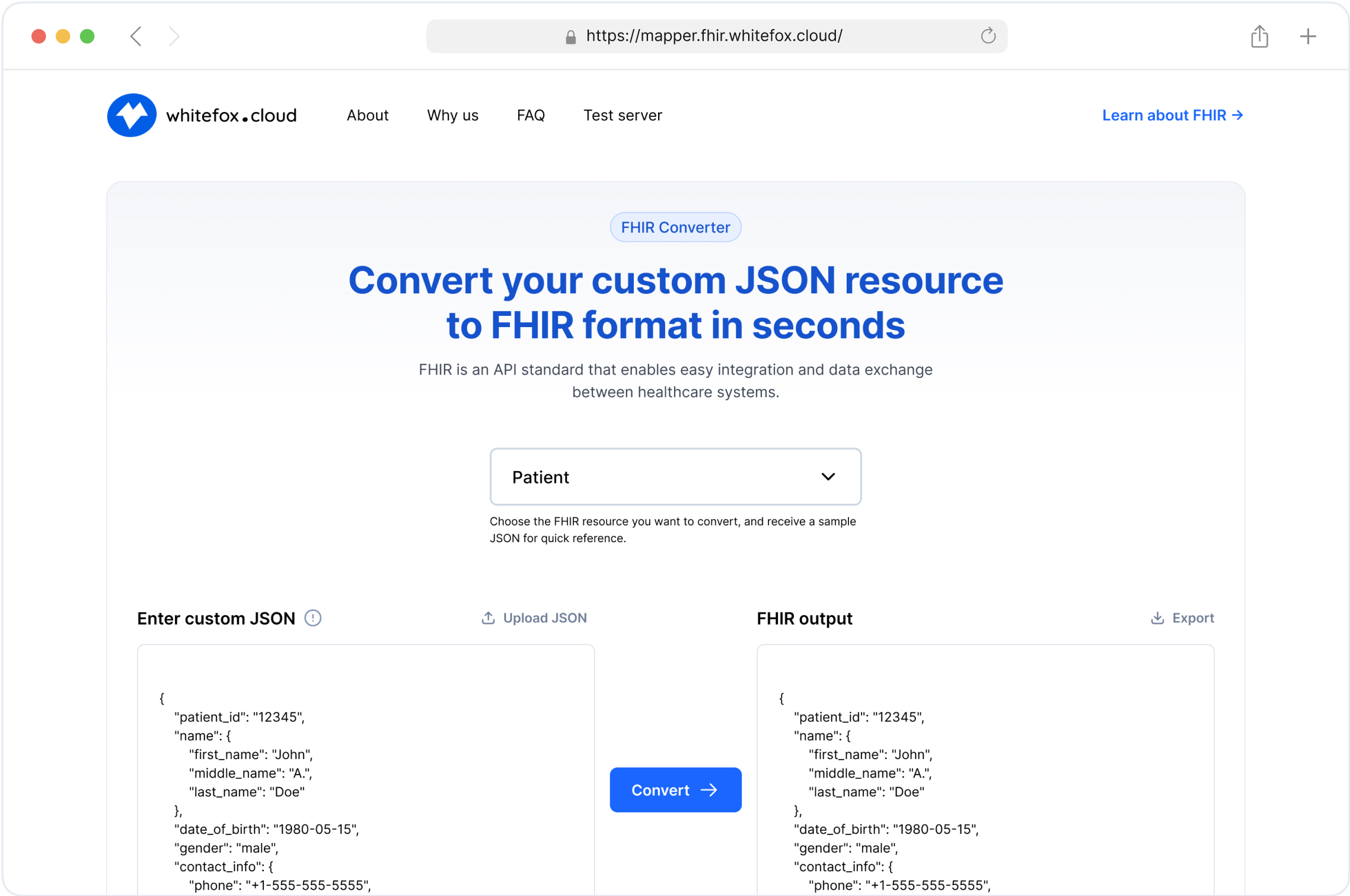
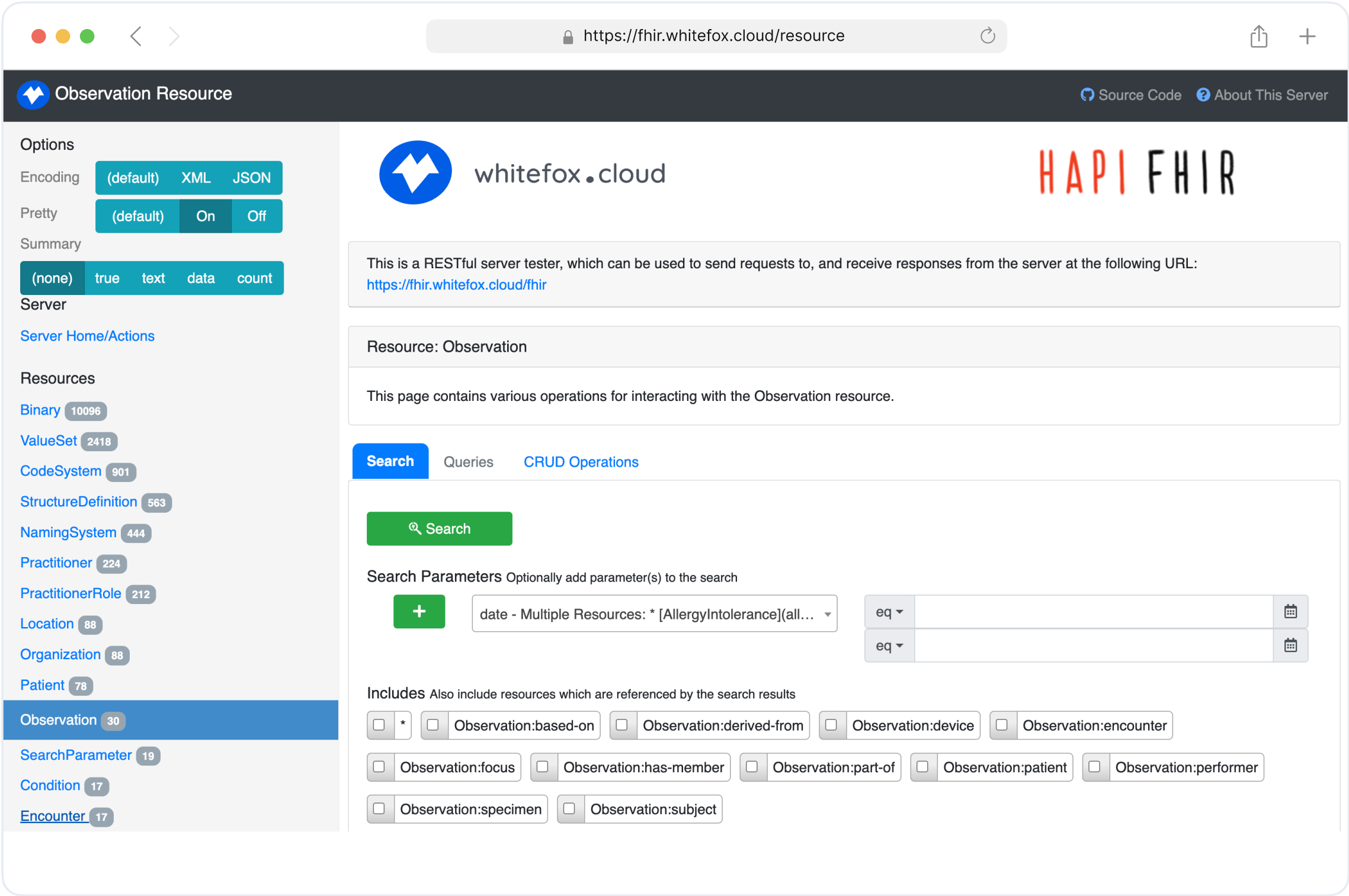
Simplify Your FHIR Integration with Our Free Tools
Streamline Your FHIR Implementation
We offer comprehensive FHIR services, from consultation to ongoing maintenance. Our Healthcare Software Development Services